

Volume 22, No. 2, Art. 16 – May 2021
Canadian Football League Players' Reporting of Concussion Symptoms
Daryl William Harrison Stephenson, Elizabeth Anne Kinsella,
Jeffrey David Holmes & Andrew Malcolm Johnson
Abstract: Self-reporting of concussion is essential to appropriate intervention, and failure to report concussion-like symptoms is a significant issue. In the current study we sought to investigate factors that contribute to the process of self-reporting concussion symptoms within the context of the Canadian Football League. A constructivist grounded theory methodology was adopted, employing in-depth, semi-structured interviews with ten Canadian League Football (CFL) players. We found significant complexity within the decision-making process for CFL players, when assessing whether or not to report a concussion. In the preliminary grounded theory emerging from the study, we identified two stages involving 1. pre-game preparation, and 2. assessing the impact. In addition, we determined three related processes (themes): 1. intrapersonal symptom checklists, 2. perceived pressures to play, and 3. certainty of symptoms.
Key words: concussion; football; reporting; underreporting; grounded theory methodology; interviews
Table of Contents
1. Introduction
2. Materials and Methods
3. Results
3.1 Stage 1: Pre-game preparation
3.1.1 Intrapersonal symptom checklists
3.1.2 Perceived pressures to play
3.1.2.1 Job security
3.1.2.2 Importance of the game
3.1.2.3 Athletic identity
3.2 Stage 2: Assessing the impact
3.2.1 Certainty of symptoms
3.2.1.1 Self-assessment strategies
3.2.1.2 League and team trainer intervention
3.2.1.3 Teammate intervention
4. Discussion
5. Conclusion
A sport related concussion (SRC) is described by the Berlin concussion consensus statement as a traumatic brain injury induced by biomechanical forces (McCRORY et al., 2017). A variety of other terms are also used interchangeably with concussion, such as mild head injury, mild traumatic brain injury, and cerebral concussion (ANDERSON, HEITGER & MACLEOD, 2006). Concussion, however, is a frequently used terminology for describing brain injuries in sport settings, with sport-related concussion (SRC) also commonly used within scientific studies (VENTRESCA & McDONALD, 2019). Impacts to the head, or to the body that transmit force to the brain can cause concussion (McCRORY et al., 2017). As such, protective helmets and equipment can never fully protect a player from concussion (GOLDBERG, 2008). With increased intensity in competitive sport, concussions are an ongoing problem for athletes, particularly in American style football (KERR et al., 2019). Concussion symptoms can linger and change the life-course of a football player (FURNESS, 2016; MANLEY et al., 2017). GUSKIEWICZ et al. (2005) illustrated that National Football League (NFL) players had an earlier onset of Alzheimer's disease. Furthermore, players with three or more concussions were five times more likely to report mild cognitive impairment and showed a threefold prevalence of memory problems compared to players who retired without a history of concussions. NFL players are at three times the risk of developing a neurodegenerative disease compared to the general public (LEHMAN, HEIN, BARON & GERSIC, 2012). While undergoing concussion symptoms, a second impact can be devastating, and can even lead to death (MAY, FORIS & DONNALLY III, 2020). Given that recovery from concussion can take a considerable amount of time, second-impact syndrome is a noteworthy problem. Second-impact injuries can occur between games and practices, underscoring the importance of reporting and managing even "minor" concussions. Concussions also pose a risk of further musculoskeletal injuries (MSK); athletes with a concussion history are at double the risk of sustaining a MSK injury (McPHERSON, NAGAI, WEBSTER & HEWETT, 2019). [1]
While concussions cannot be fully prevented without drastically changing the sport, which would be met with considerable resistance, the management of suspected concussions can be improved. This task necessarily falls to players, trainers, physicians and coaching staff, who must identify and report symptoms, implement evidence-informed interventions and protocols, and carefully monitor return to play. While this is the job of trainers and physicians, changing the culture of concussion reporting to one that causes players to identify teammates' concussion symptoms at an earlier stage could make a difference. One difficulty is that failure to report concussion-like symptoms is a known problem, and the reasons why players fail to report are not yet fully understood. Concussions are largely invisible injuries. Therefore, assessment requires athletes to report the symptoms before an evaluation can occur. As these assessments frequently occur on the side-lines during a game, players can sway diagnostic decisions based on what they say (or do not say) to the physician. MEIER et al. (2015) found that athletes self-reported significantly fewer symptoms when a formal test was used compared to self-reported symptoms collected confidentially. In recent years, the trend has been to take players to a private area such as a locker room to be evaluated, with the player either re-appearing ready to play or not. In the NFL since 2016, it has been a rule that players must be removed from the field to be evaluated and must also be accompanied by medical staff. Heavy fines are set for teams which do not follow these protocols. The King-Devick test has been used by the Canadian Football League as a sideline concussion test; the test is used by team trainers to evaluate function by capturing eye movements and time to perform rapid number naming (GALETTA et al., 2011). The test has been shown to be a reliable measure (NAIDU, BORZA, KOBITOWICH & MRAZIK, 2018). To take the test, however, a CFL player needs to self-report symptoms or be identified by league officials or team trainers. [2]
In a 12-year study of the NFL, CASSON, VIANO, POWELL and PELLMAN (2010) found an incidence rate of .38 to .42 concussions per team per game. In 83.5% of the concussions reported, players returned to play with no missed games or practices. From 2009-2015, KELLY (2017) reported an increase in the number of concussions in the NFL, while also showing that certain teams reported a lower number, likely due to underreporting. Underreporting is common in many professional sports. For instance, 17.2% of elite rugby players in Australia chose not to report concussion-related symptoms in 2018 and 2019 (LONGWORTH, McDONALD, CUNNINGHAM, KHAN & FITZPATRICK, 2021). In a study with professional rugby players in Ireland, forty-five percent of players reported at least one concussion during the season, but only 46.6% reported it to the medical staff (FRAAS, COUGHLAN, HART & McCARTHY, 2014). The reasons included not thinking the injury was serious, not wanting to be removed from the game, and not wanting to let teammates or coaches down. [3]
Failure to report has also been found in college and high school athletes. In high school football in the United States, it was shown that up to 50% of concussions go unreported (McCREA, HAMMEKE, OLSEN, LEO & GUSKIEWICZ, 2004). In a study of high school athletes of different sports in the United States, only 40% of concussion events and only 13% of short-lived concussion events were reported (REGISTER-MIHALIK et al., 2013). MOREAU, LANGDON and BUCKLEY (2014) demonstrated that in the National Collegiate Athletic Association in the United States, student athletes did not always report concussion symptoms, and were dishonest when reporting ongoing symptoms, sometimes out of fear of failing to meet teammate expectations. CHRISMAN, QUITIQUIT and RIVARA (2013) identified factors such as not wanting to stop playing, looking weak, or letting teammates down as contributing to underreporting in a study of high school athletes. Athletes have also been shown to have difficulty differentiating concussion symptoms and other etiologies such as dehydration or viral illness (ibid.). Authors of a large systematic review of adolescent athletes and under-reporting discovered that athletes desired to remain in games and that interpersonal dynamics with teammates and coaches acted as barriers to reporting (PENNOCK, McKENZIE, STEACY & MAINWARING, 2020). [4]
In a Canadian Football League (CFL) survey, 44.8% of players reported experiencing symptoms of a concussion during the season, 69.6% reported repeat concussions; yet only 18.8% recognized they had a concussion (DELANEY, LACROIX, LECLERC & JOHNSTON, 2000). DELANEY et al. noted that in a prior study, players reported their reluctance to answer truthfully for fear it would jeopardize their chances of making, or remaining with, a team (p.13). They recently reported that 82.1% of CFL players who suspect a concussion do not seek medical attention, noting that players commonly do not report concussions due to perceptions that the episode poses little or no danger (DELANEY, CARON, CORREA & BLOOM, 2018). This may be due to comparisons with concussion episodes in the past from which they recovered (ibid.). [5]
Given the high rates and dangers of concussion in sports like football, that self-reporting of concussion is essential to appropriate intervention and care, and that failure to report concussion-like symptoms is a significant issue, we sought to investigate factors that contribute to the process of self-reporting concussion symptoms within the context of the Canadian Football League. The research question was: What factors contribute to the process of reporting concussion symptoms in Canadian Football League players? [6]
We will begin by defining the methodology and focus of the study, followed by an introduction of the positionality of the researcher involved in collecting and analyzing the data. After that we will state the sampling methods used to recruit participants for the study, and discuss the data collection techniques that took place between August 2017 and June 2018. We will then discuss the data analysis process that shaped the results. The results section is next, starting with an explanation of the grounded theory, followed by an examination of the themes and subthemes involved in the stages and processes. After the results, a discussion elaborates on the findings, and ends with a conclusion. [7]
For this study we used constructivist grounded theory methodology (CHARMAZ, 2014). The aim was to advance knowledge about factors that contribute to CFL players' reporting of concussion symptoms. A secondary focus was to highlight social processes that may shape CFL players' decisions and approaches to reporting concussions symptoms. All materials and methods employed within this study were approved by a University Research Ethics Board. [8]
The first author was a CFL player for six years and sustained two concussions during his career. He was a football player from the age of six and likely sustained concussions and minor concussion-like events earlier in life that went undiagnosed. Admittedly, he also "played through" injuries and was not educated about concussions early in his career. [9]
Being a CFL player with lived experience of concussion shaped the researcher's positionality and capabilities as a researcher. Given his knowledge of the context, the first author attempted to enter the research with an open mind (BRYANT, 2009), to recognize that both researcher and participants bring pre-existing experiences to co-create knowledge, and to be aware and reflexive about how being an "insider" can shape the social dynamics in the interview process in various ways. The first author also engaged in reflexivity and examination of assumptions, and did not presume to know about the concussion experience of other players. The researchers undertook a literature review in advance—which can be controversial in grounded theory methodology—however, care was taken not to force preconceived ideas onto the findings, and to use the review to inform theoretical sensitivity. [10]
Purposive sampling (PATTON, 2002) was used to recruit ten current and retired CFL players to the study. Theoretical sampling was not used due to the specificity and limited number of potential participants. Although theoretical sampling pointed to the ideal of also interviewing CFL players currently living with concussion, our local ethics board did not approve inclusion of these participants due to ethical concerns. Further, due to potential concerns about coercion, interested participants were required to contact the research team, rather than being recruited to the project by the researchers. Participants were either diagnosed with a concussion during their career or had experienced unreported concussion-like symptoms. Participants were male, between 20 and 32 years of age, with various levels of experience ranging from first year to one player who had been retired for four years. Participants were ethnically diverse, Canadian or American citizens, and played various positions. Individuals currently in treatment for concussion were not included. [11]
Recruitment involved contacting gatekeepers who had access to potential participants through the CFL and the CFL Players' Associations, and asking them to inform players to contact us if they had experience with concussion or concussion symptoms. Coaches, players, and agents reached out to players, and these individuals contacted the primary researcher and consented to participate. Participants were currently: 1. playing, 2. recovered and playing, or 3. retired and not playing. Participants appeared to want to discuss their experiences. They may have been more comfortable participating given that confidentiality was assured, and knowing they would be speaking with a former CFL player. [12]
Typical of constructivist grounded theory methodology, semi-structured interviews were employed (CHARMAZ, 2002). Questions focused on CFL players' experiences with concussion symptoms and the process of reporting or non-reporting. The interviews included open-ended questions and permitted us to follow lines of inquiry that emerged during the interviews. Participants were interviewed in person, by Skype, or by phone, and all interviews were audiotaped. Telephone and skype interviews are increasingly common in qualitative research and have produced comparable results to face-to-face interviews while providing benefits such as not needing to travel (OLTMANN, 2016). In-person interviews were conducted at the participant's home or location of choice. Interviews averaged 30 minutes. Memo writing involved creating analytic, theoretical and conceptual memos about insights and questions; these memos informed data analysis and team discussions (THORNBERG & CHARMAZ, 2014). [13]
Data analysis occurred throughout and after the data collection process. Common to grounded theory methodology, data analysis involved breaking the data into smaller sections, then coding and organizing the data according to patterns (EVERS, 2016). Initial coding involved labeling segments of the data (THORNBERG & CHARMAZ, 2014). Focused coding was iterative and involved interaction with the data, and with other codes, participant discussions, and revisiting the research question. The constant comparative method was used, i.e., constantly comparing data, codes, contexts and categories that fit the data, and identifying patterns. While emergence can be a problematic methodological concept, patterns did emerge that were not anticipated prior to the interviews. These patterns were then used to develop leads for future interview questions. Meetings between the first author and the research team brought critical reflexivity from multiple diverse perspectives to the emerging interpretations. Many grounded theory methodologists suggest that when data are collected and compared, patterns are found, and when no more patterns arise, saturation is said to occur. Toward the end of data analysis, patterns were repeating themselves and no new patterns arose (THORNBERG & CHARMAZ, 2014). NVivo 10 software was used to transcribe, code, and manage the data. Subthemes were combined to develop three themes that encompass the main factors in the process of reporting a concussion. Stages of the process were identified. [14]
A preliminary grounded theory was generated through the analysis process that depicts stages and processes of CFL players' decisions to report a concussion. The grounded theory is comprised of two stages, and three overarching themes, shaped by several subthemes. The themes occurred with each player, while the subthemes varied between players. Although presented separately, the themes and subthemes are interrelated and intertwined. The grounded theory is illustrated in Table 1.
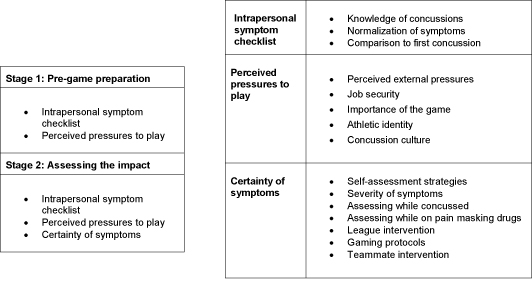
Table 1: Reporting of concussion symptoms: CFL players' decision-making processes [15]
The processes occurred across two stages: "pre-game preparation" and "assessing the impact." Pre-game preparation takes place before contact on the field has occurred. At this stage "intrapersonal symptom checklists" and "perceived pressures to play" were seen to shape players premeditated thoughts about concussions including their knowledge, attitudes, and expectations. "Assessing the impact" involved the players' thoughts and strategies, and assessment of their concussion symptoms immediately following an impact. This stage involved consideration of the "intrapersonal symptom checklist," "perceived pressures to play" and "certainty of symptoms," and was shaped by several subthemes, some of which were involved in the first stage. [16]
The grounded theory depicts a process whereby players engaged in an internal evaluation between assessment of the impact, and their pre-game thoughts. Players self-assessed concussion symptoms and attempted to be certain of their symptoms. Their level of certainty was shaped by their intrapersonal symptom checklist, and their decision to report was influenced by their certainty of symptoms and perceived pressures to play. This resulted in players evaluating the risks of continuing to play and deciding whether to report a concussion or not. [17]
3.1 Stage 1: Pre-game preparation
3.1.1 Intrapersonal symptom checklists
Many participants appeared to have an intrapersonal symptom checklist of what a concussion experience would look like. This checklist was unique to each player and involved several factors, including their knowledge of concussions symptoms, their normalization of concussion symptoms, and the comparison to previous concussion symptoms. Players referred to an inner checklist to anticipate what a concussion would look like, while assessing themselves, and to decide whether to report. [18]
Normalization of concussion symptoms was a major subtheme within the intrapersonal symptom checklist, which also impacted the self-assessment theme. Normalization was aligned with comparisons to the first concussion, severity of symptoms, athletic identity, pain masking drugs, teammate intervention and concussion culture. A number of participants seemed to normalize symptoms rather than report them, with symptoms like headache and neck pain viewed as a common side effect of football. One participant (5) described how he played an entire season with weeklong headaches.
"'Oh, there's that same headache again. No big deal kind of thing.' I guess that was my thinking ... I was pretty much going through a cycle each week ... I would have like crippling headaches for our off day ... And then game day I'd feel OK. And then obviously I'd go and hit people during game day, and it'd be like a constant cycle of that. So, I pretty much went through 22 weeks of that, and it didn't ... feel great ... that year was a tough one ... we had a new head coach ... so I was going to prove myself." [19]
Normalization appeared to be connected with the severity of concussion symptoms. Participants discussed symptoms needing to be severe or drastic enough to cause alarm, otherwise they were seen as normal or as part of the game. A number of examples were expressed by participants.
"It has to be bad to the point where you literally are out of it, and like the next day you're not feeling right. And that's where like the guy I mentioned two years ago [teammate] ... he didn't feel right the next day. Like that was like, man, like 'I literally got to report this.' So, I think we're all ... like ... how bad is it when I self-assess myself and then we need to be true to ourselves" (Participant 7). [20]
Participant 5 normalized symptoms by comparing concussion-like symptoms to any kind of injury, suggesting that it has to be "really bad" to be reported:
"Same way with any injury—like if you were to hurt your wrist ... 'well it's my wrist' kind of thing ... 'should I just kind of put a brace on it or tape it up and just like keep going.' So I think, concussions are the same in that respect and that ... you really have to be really bad [to report]." [21]
Another player (9) normalized certain concussion-like symptoms by suggesting he would "wait it out" and "live with it":
"Yeah. I would wait it out because usually ... especially in the migraine, like, I know what it does to my body, so the next day is usually still not the greatest ... So either the next day, or the day after, like if it's still like a lingering headache, or like my eyes are really sensitive to light, then I'd be like 'okay I should probably go and talk to my trainer, make sure I'm not concussed.'" [22]
Participant 7 indicated he would wait until the next day to see if something is still going on, implying that a day or two of headache, pounding, nausea and migraines are normal:
"If I feel the effects after the game, if my head is pounding, like migraines, like you know, like just me not feeling comfortable after the game. I think it would be a huge tell, like the next day if it's like OK. Because ... it's one thing to be sore after a football game, but if my head is just like feeling nauseous or something [the next day], then I would feel like 'OK, there's something going on.'" [23]
Connected to the idea of severity of symptoms was the discussion that the loss of function, wobbly feelings, or disequilibrium was not a normal symptom, and therefore would result in the recognition of a concussion. One participant (2) highlighted how he would not have reported if his function was not affected: "You never want to pull yourself out of a game. You know, as long as I was functioning, and wasn't taken off the field, then I don't think I would have said anything." Another participant (6) noted how it scared him when his balance was affected: "Yeah, what scares me is when I have wobbly legs ... cause the first time I had wobbly legs I knew something wasn't right." Despite being aware of concussions, Participant 1 recognized losing consciousness or memory as a sign of concussion, with less dramatic symptoms depicted as normal:
"I feel like I was pretty aware of the whole concussion thing and I guess for me it was always, like, take a second and, like, see how I feel, or if I come to, or if I feel normal within a few seconds I was okay, you know. I think for me if I been knocked out, woken up, and not remembered anything, then I was like 'okay I got a concussion'—but anything that was semi-okay then I was like, 'oh it's not a concussion,' or 'I'm okay.'" [24]
Short-term concussion-like symptoms were labeled and normalized in various ways such as "getting your bell rung," "ringers," or "being shook up." Participants struggled with identifying concussions when symptoms could overlap with short-lived concussion events.
"Yeah, things like having your bell rung, being shook up, or just having a headache you know from a hit or from a game ... it kind of came along more of the territory... you know you're going to get hit ... you remember getting hit... and it's just... what happens. You get your bell rung, you carry on and you keep playing" (Participant 2). [25]
Younger participants appeared more aware of the potential for these events to be concussions. Older players seemed to be aware, but some admitted that they were less aware in their early days: "As far as a concussion ... I thought a concussion is that you were knocked out cold, had to be helped off the field, or carried off the field" (Participant 2). These short-lived events were reported by every participant. Some players waited them out for a short amount of time and then monitored their own symptoms. When the symptoms cleared, they were ready to go, and assumed the hit did not result in a concussion.
"There were a couple times where I felt like I was on the edge of being concussed...but it went away so quickly like if I got my bell rung, while I was low on oxygen, and you just kind of spaced for a second. My first thought is, 'uh oh, I'm going to enter that state of being concussed where I'm just lost,' but a couple times it quickly subsided, and I was right back to normal, no headaches or no ill effects. Now I'm sure arguably there is some damage on some level, but I was right back to normal" (Participant 1). [26]
Players' comments pointed to the normalization of concussion symptoms within the culture of the sport. One participant (7) noted that "it's the fact that you hear it all the time. My head is spinning, my head is hurting—my head!" that contributes to this normalization, and turns it into "not that big of a concern," suggesting that "if the guy was, like, literally like bleeding out of his nose ... I'd be like ... we definitely have to address this issue" but otherwise heads spinning, and hurting were relatively normal. Not only did symptoms appear to be normalized, but some players shared stories of how that led to the gaming of concussion protocols. A few players talked about "gaming" the concussion protocol pre-emptively as something they had noticed or done themselves. Participant 4 talked about tricking the protocol.
"But I'm a smart guy. It's not hard to trick the protocol. They asked you to remember certain words. It's like cat roof something else you know money, knife, and bag or something. I just recited the words, and ... by the time they asked me again, I knew what the words were. So I went back and played." [27]
The underlying cause of wanting to game the protocol seemed to be the belief that the player did not actually have a concussion. Some disagreed with this practice:
"Some guys can hide it well. Now you also get some guys be, like, 'oh, I'll make sure I kind of dog it a little bit on my concussion test, so if I ever do get rocked, and I write it, then I'll be okay.' Straight up, I've heard people say it and I'm like, 'OK, bro, you do you. It's your brain, it's your life'" (Participant 9). [28]
Normalization of concussion symptoms was also aligned with the assumption that concussion symptoms would be similar to previous experiences. Many participants expressed impressions that symptoms of a new concussion would be similar or the same as previous concussions. Participants discussed thinking back to previous experiences to assess whether the current injury was indeed a concussion. For example, if they blacked out in their first concussion, there seemed to be a predisposition to think that they would black out again if they sustained a concussion. An attitude of "this is the way concussion looks for me" was prevalent. For instance, Participant 6 stated: "It crossed my mind [that I had a concussion] but I was like 'nah,' cause if the other one is mild, this one doesn't even feel like that one," whereas Participant 1 indicated "the symptoms were the same for me every time." [29]
3.1.2 Perceived pressures to play
When asked about external pressure to play through injury or concussion, many participants discussed that it was mainly internalized or perceived pressure that drove them to return to play. As Participants 6 and 5 stated "No, I don't feel any pressure at all. I feel pressure on myself, but no pressure by the club," "I guess overall, like, pressure for myself to perform. Pressure ... to not let your teammates down, and then pressure to prove yourself to your coaches." Participant 1 discussed the possibility that external pressure was also internally constructed.
"I would want to say external pressure, but not necessarily. It can be internal. So I think 'I don't want to let my teammates and coaches down,' and I know they, you can tell in their voice, their tone, that 'hey how you doing?' underlined with 'you know when you coming back?' ... So, there is external [pressure], and maybe that's internally interpreted." [30]
One participant (4) discussed coaches understanding players' situations and that they could act as positive influences to remove pressure.
"They [the coaches] know, if you hit someone or you get it, they know, they know, they'll be like, 'Yo, like you, you took a hit, like are you alright' they know what you are like, they know you feel pressure to keep going. So like, you know, 'you just kind of watch from the side, we want you ready for the game so you can take a little bit of time.'" [31]
Job security was identified as a subtheme of the perceived pressures to play. Several participants expressed fear related to losing their place on the roster or losing their job as reasons not to report concussion. As one player (9) stated: "more in fear... like, if I get hurt, once my injury's gone, they don't put me back in, and they just let me go. And I lose my job." Another player shared: "And then halfway through the year I got traded. So, I obviously wanted to prove myself ... I felt like if I took a seat on the bench ... I would lose my job" (Participant 5). [32]
A number of participants discussed their perceptions of a limited window within which to showcase their skills and secure a position. Accordingly, participants discussed being willing to hide concussion symptoms and injuries, rather than lose playing time or opportunities to prove themselves or achieve their goals. Rookies seemed to experience more job insecurity given less time to establish themselves. Participant 7 described how his actions would have been different if he had been more established:
"If I was an established vet, I wouldn't be practicing ... I would like immediately go to the trainers ... it's just the fact that ... I'm there to establish myself, and trying to make a name for myself, and I think that goes for anything ... You can't just jump to the wheel and say, 'Hey, I'm taking a couple of days off.' Like it's not gonna work like that." [33]
On the other hand, a more established player (3) spoke about the bigger picture, and being more inclined to report concussion-like symptoms: "yeah, at this point ... I see there's a bigger picture now. Earlier in my career I was probably too much of a meathead to be like, yeah, I got a concussion." Participant 8 reflected on responding as a rookie compared to as a veteran.
"The more you gain a relationship with the trainers and stuff, I think I would come out and tell the trainers, but when I was young and hungry and you never know if you're going to be on the roster ... I might be more hesitant and want to get more plays and chances on the field to show my skills." [34]
Given the implications for play time, and one's career overall, many participants reported being unwilling to report a potential concussion.
"You think you have it [concussion] ... they are liable. They have to say you have a concussion. So, you have to weigh those options. Right? 'Can I go through this?' 'Do I need a rest?' ... It puts pressure on you... like 'How's it going to make me look?' 'What does that mean for my career?' ... 'How many games would you be out?' 'What does it mean for your pay check?' 'What does that mean for your playing time?' 'What does that mean for your stats and your aspirations and your goals?' ... It's a big picture thing" (Participant 4). [35]
3.1.2.2 Importance of the game
Perceived pressure to play was also related to perceptions of the importance of the game to the team, or for the individual's career milestones or contractual goals. The importance of the game for the team frequently factored into decision-making. Helping the team win crucial games or playoff/championships was identified as motivation to fight through pain and injuries, in order to participate. As Participant 3 explained, these factors can influence a player's willingness to gamble on a worse health outcome for a better outcome of the game: "It's like high-risk, high reward, people go play the roulette tables every day." The importance of the game was highlighted as a reason to play through symptoms.
"You're just gritting your teeth at that point. This is the biggest stage... getting in the league is one thing but getting to the big dance, and you have a concussion. Man, they might have to knock me out. I'll deal with it later" (Participant 6). [36]
The importance of the game also had the potential to influence coaches and team staff to allow a player to return to play. There is a connection here with the subtheme of "concussion culture," the theme of "certainty of symptoms," and the subtheme of "gaming protocols."
"He got super rocked. It looked like he passed out. It looked like he got knocked out. And then he got up and ran off and I don't think they did anything because it was a playoff game and they needed him. That was a situation where I was like 'Damn. You guys are really just going to let him do that?' But he's the guy and he wants to play ... 'Woah, alright.' ... sometimes they're on it and then other times you're like, 'oh, well we need him to play, he's good' and that's it'" (Participant 10). [37]
Career milestones or contract details such as bonuses also contributed to perceived pressure and influenced participants' decisions to play through a concussion. One participant (2) commented on how playing in the CFL was the realization of a lifelong goal, creating a situation where players may gamble on playing despite concussion symptoms.
"From when I started in high school, you're always kinda striving for the next thing, whether it's the next game, or whether it's to go on to college, or go on to pro. And there's always the next thing, and I think in the CFL, you know you're always trying to pave your path and make your name for it. And I think each year, it was just kind of a chance to prove yourself to the league, to your team, to your coaches, to yourself. Just constantly striving for that next plateau, whether its personal or team oriented." [38]
The importance of the game to players themselves, in the sense of loving their sport and what they do, was another factor that shaped reporting.
"But it's like ... when you hear about the effects of alcohol and tobacco, but you're an alcoholic or a chain smoker, it sucks because you realize the truth is right there in front of you, but you're like, I love this sport and this sport is my career. Now what do I do? A lot of guys were put into that line where it's like do I just stop playing right now? (That) was really the hardest part of it" (Participant 8). [39]
Participants discussed trying to find a balance between limited time to prove oneself, especially as a starter, but also not performing under compromised conditions where one's reputation could be tarnished by playing with a hidden injury. While a "tough it out" concussion culture was evident, it was also discussed that coaches accepted and reinforced not playing when severely injured, not just because of the potential for further injury, but also due to the risk of tarnishing game films and hurting the team goals. This aligns with subthemes that discuss players' self-assessment of the severity of the symptoms, maintaining job security, and considering team goals as priorities over concussion management. [40]
Another perceived pressure to play was related to maintaining one's athletic identity, most notably as a resilient and reliable player. Many participants seemed to have an idea about their identity as a tough resilient player who would play through injuries. Participant 9 described "I've always been like prideful, like um, I'm a tough guy. It doesn't matter what you do to me, 'I'm going to play,' type deal." Players described battling through injuries and being praised for being "tough" and "reliable" athletes. This identity seemed to influence how some players approached their recovery. As Participant 2 stated:
"It's that fine line of, like, you don't want any injury, or possible injury ... or concussion, to taint your credibility as, like, a reliable or tough individual. And if you are ... taken out of the game, it kind of goes against your identity, or your ability to be reliable, to be counted on." [41]
However, this was not always the case, as other participants expressed how they valued their long-term health and discussed what they would do to come out of a concussion in a healthy way.
"My competitive edge will tell me to go. But I also listen to the doctors. Yo, my health is number one. You know, like, I don't have any kids, but if I had kids, I got to think about them. It's not all about me, you got to think about your family, and what's best for them too" (Participant 6). [42]
Participant 4 noted that the "tough" guy identity was perhaps related to historic football culture, but that it was possibly changing to become more health conscious over time: "At that time it was, we were still in that era of like 'be tough ... this is what happens in football'." Similarly, Participant 10 stated: "I'm sure I did [have the tough it out mentality] ... that's what it was when we were in high school. Just, like, 'suck it up, be a man, play ball.'" [43]
3.2 Stage 2: Assessing the impact
Certainty of concussion symptoms is a theme that was frequently discussed. When participants assessed symptoms, they looked for certainty before disclosing or reporting a potential concussion, yet certainty was not clear cut. Consideration of the symptoms through an inner checklist, and the tendency to normalize symptoms (as discussed earlier) came into play during the assessment process. [44]
3.2.1.1 Self-assessment strategies
Players self-assessed their symptoms and considered the chance of concussion. Self-assessment strategies were highly individual, and many different factors were considered and strategies used. In cases where the CFL does not intervene when a player undergoes a direct impact to the head, it is up to the player to self-assess and decide whether to report a concussion or not. All participants described how they drew on their knowledge to self-assess for concussions. This knowledge appeared to be influenced by factors discussed earlier such as the intrapersonal symptom checklist, the education provided to all players in the CFL, the tendency to normalize symptoms, and assumptions that symptoms would be similar to a previous concussion experiences. [45]
Participants noted a range of timeframes for initial symptoms to clear, ranging from 10 seconds to around 1 minute. It was interesting to note participants' assumptions that these events would take a certain amount of time to subside, or that steps could be taken to alleviate the symptoms. As one participant (6) stated: "Yeah, like I'll take some hits or whatever, or I'll take a hit and I'll be a little bit blurry. I'll literally just shake my head, or like close my eyes, or like put water on my face and just wake up. And I'm ready to go." They reported strategies to self-assess concussions, such as attempting to remember information such as times and dates.
"I've made tackles where it's like, I make the tackle and it's kind of like my ears are ringing. It takes a second just to kind of shake it off, and then snap back to it and I just keep going ... I actually run through the date and time, the score of the game, I just try to see if I can remember, like, those little things, and I am usually all right" (Participant 10). [46]
A number of participants discussed assessing the physics of the contact. One participant (4) suggested that he would be more cautious if he received a big hit than if he were the initiator.
"I might have made the hit, and then been like, 'oh shoot.' Like I hit that guy really hard. Like I rattled myself, and then just kinda shake it off. Um, but if I got it, it would have felt a little bit like, 'man, I got lit up.'" [47]
Many participants indicated that it is difficult to determine whether one has concussion symptoms, noting that some symptoms could be due to other causes such as illness or dehydration. As Participant 8 described, when he was "nauseous" following a hit, his tendency may be to attribute it more towards "heat exhaustion, or over-heating" rather than concussion. A complicating factor adding to the uncertainty is that players may be concussed, which may impact their capability for clear judgment: "The state of mind you're in, you're in no state to assess the risk" (Participant 1). [48]
Adding to the assessment complications was the discussion that many players were also taking pain relieving drugs; either for the whole season or for particular games or practices. Pain masking drugs can interfere with players' perceptions of the severity of symptoms, and consequently with abilities to recognize and report symptoms. Toradol is a common pain killer that most participants discussed using at some point. Participants also indicated that they never factored pain killers into the equation when assessing concussion symptoms. Pain killers are given to players by the team trainers, but nothing prevents them from taking them on their own before games or practices. As Participant 7 discussed: "Like, I feel amazing ... I can play again, so I wouldn't factor it [concussion] in, just because of my experience with Toradol and how it helped me." Participant 3 stated: "Like [people] used to pop Toradol, like 'just let me get a Toradol, we're going to war.' Like nothing could hurt you. Get me one of those because when it does (hurt) I don't want to feel it." Similarly, Participant 8 stated: "So, I would take Toradols and those were like the wonder pill ... I never would have thought, 'okay, I'm on these painkillers, maybe I should be extra cautious about concussion symptoms.'" [49]
Participants also expressed uncertainty regarding the risks of returning to play. This added further complications to the process of reporting symptoms. Some players assumed they would be fine, but also recognized some level of risk and were uncertain as to whether continuing to play would cause more damage. For several players, this uncertainty contributed to risk-taking and "playing through symptoms." For instance, when asked "Would you be concerned playing through symptoms?" Participant 1 responded:
"No, and I'm one of the last people that should be saying no, because I've studied some of the effects... But to me, I don't have enough clarity on the confirmed results, or outcomes of getting multiple concussions, and so there's no definite answer. I don't know ... there's no equation. It'll probably get worse, and you could probably do damage, but we don't know. So, [players] usually take the poor choice, and go back in." [50]
Due to uncertainty of the risks associated with play, many participants described playing through symptoms. Participant 9 described a dramatic hit that resulted in "seeing stars," "losing vision," and "everything going black" where he told his coach he "just needed a sec," and then he returned to play.
"There's actually been times in a game where, like, I hit somebody, and then I saw stars, and everything went black for a minute, and then I kinda came to and kept playing. My first thought was 'wow, shit, the ground was hard.' ... my head just went boom. And I like stood up right away, and I just had, like, the stars come, and everything went black and I kind of walked to the sidelines without being able to see ... I listened for my coach ... I could hear his voice. He asked me 'what's wrong with you?' I was like, 'nothing, I just need a sec' ... And then once I came to, once I could see again, I was like 'okay, I am good.'" [51]
The invisibility of concussions, and uncertainty regarding severity were noted as contributing to playing when symptoms were present, with implications for reporting. When asked what may concern you about coming forward with your concussion symptoms, Participant 5 stated:
"Concussions aren't one of those things that you can [see], you can point to a broken bone and be like, 'see, it's broken,' but concussions are one of those things that you can't, I mean, you can go through testing and stuff, but there's no real way to prove how bad it is and how bad you're feeling. So, if I was saying like, 'I'm constantly having headaches,' ... I didn't think that would be enough of a cause to take some time off, either practice or a game." [52]
3.2.1.2 League and team trainer intervention
The CFL spotters or the team's trainers could also intervene at the assessment stage if they witnessed an impact of concern. The players discussed how this intervention was effective at identifying players with concussion-like events and removing them from play.
"Yeah. I think they are better with the protocols, I think that informed us a little bit better about what we're looking for, as far as, like, people assigned to looking for concussions now. They see one sign they take the guy out right away" (Participant 6). [53]
The shifting culture toward interventions when concussions are witnessed, and players' recognition of concussions being taken more seriously, was discussed.
"But like a sprained ankle, or wrist, or you know, anything little like that. It's like, 'OK, dude, it's a sprained ankle. Tape it up, let's play.' Concussions are concussions. Like, if you have symptoms... I'm pretty sure they shut you down for a minimum 2 weeks now" (Participant 9). [54]
One participant mentioned that the league sometimes seemed overly concerned, and that after every big collision players are sidelined for concussion tests.
"As soon as there is any helmet-to-helmet contact ... your trainer comes up to pull you aside, and get you a sideline conky test, to make sure that you're OK. They are very on top of it right now... I have a guy blindside me and I'm like, 'agh shit,' you know what I mean? ... You go to the sideline, they're like, 'Hey, take off your helmet' ... 'we have to make sure you don't have a concussion' and I'm like 'I'm fine.' 'Well you have to do it.' 'OK, do it. I'll be fine and keep playing'" (Participant 9). [55]
Despite feelings of annoyance, Participant 9 agreed that these strategies were necessary, to combat hiding of concussions, and for player safety. Participant 6 concurred:
"I blacked out for like 2 seconds, I got back my mind, and my legs felt a bit jiggly when I stood up and I was good after that. And I think I could have played the rest of the game, but they took me out of the game. But then after the game I felt. ... I was like 'man, maybe it was a good thing I didn't play,' because that night I would close my eyes and see flashing lights, I didn't feel like myself." [56]
Some participants praised the CFL and training staffs for their efforts, and the attention given to the players in concussion recovery.
"There is a lot of care given, and attention to doing the right things. If someone needed to be there, to wake you up every couple hours ... it wasn't just like, 'you have a concussion, go home and get better.' It's like 'do this and this,' there was, like, a fair bit of urgency" (Participant 1). [57]
Participants discussed their role if another player visibly showed concussion-like symptoms and failed to report symptoms. All participants indicated hope that the concussed player would initiate reporting of symptoms, and their preference to leave it to the player to initiate reporting.
"I trust them on their own judgment, because I wouldn't want somebody, if I took a big hit, and everybody was like 'are you okay? are you okay?' And then I'm like, 'yeah, I'm good.' I wouldn't want someone to be like, 'yeah, he should be on it'" (Participant 8). [58]
If an injured player was not self-identifying, participants indicated they would speak to the player about seeking help. If a player refused to report obvious symptoms, potentially putting himself in danger, participants were divided on what they would do. Most indicated they did not wish to report, for fear of jeopardizing another player's career, while some discussed that they would only intervene if the situation was severe, similar to how they made decisions to report their own concussions.
"Like, you're looking out for them but like, it's also like ... you don't want to put them in a situation where they're not playing because you told somebody. And now they're fine, but they're still not playing. You don't want to be the person to do that" (Participant 10).
"Unfortunately you could affect somebody else's job. Their livelihood, that's how they pay their bills, and feed their family, right? You would hope ... they'd be able to do it on their own, but ... I'd tell them like, 'you got to talk to a trainer' ... I personally wouldn't walk up to a trainer and be like 'Yo, this guy's rocked. You should check on him.' Unless he was like really bad, then I might have to" (Participant 9). [59]
While efforts are ongoing, participants' accounts suggest there still seems to be a perceived stigma around concussion within the CFL culture. One participant described the "stigma" of concussion as "the elephant in the room" (Participant 8). [60]
We propose a preliminary theory grounded in the data that depicts the processes of deciding to report a concussion. This grounded theory highlights two stages: 1. pre-game preparation, and 2. assessing the impact, comprised of three processes (themes) related to 1. intrapersonal symptom checklists, 2. perceived pressures to play, and 3. certainty of symptoms. We noted significant complexity within the decision-making process for CFL players when assessing whether to report a concussion, and identified a range of factors that may contribute to the reporting of concussion symptoms. [61]
It appears to us as though the culture of concussion management is progressing in a positive direction, as the CFL is currently taking steps to reduce concussive impacts. These efforts include the introduction of: annual concussion seminars, concussion symptom posters in all locker rooms, abolishing full contact practices throughout the season, use of the King-Devick concussion test on the sidelines, permission for players to obtain a second doctor's opinion, active concussion spotters looking for high impact events at each game, and a digital concussion platform (HeadCheck) to execute and monitor the effectiveness of the league's concussion protocol (CFL, 2016). Participants discussed ways in which concussion culture in the CFL has positively changed in recent years. This aligns with CFL reports that players, trainers, coaches and league officials have become more responsive, attentive and proactive in dealing with concussions over the past decade (ibid.). Football players have been reported to demonstrate greater understanding and awareness about concussion than ever before, and it has been suggested that educational initiatives are making a difference (DELANEY et al., 2018). These proactive measures need to continue and be rewarded if concussive impacts are to be reduced. [62]
Nonetheless, in our research we revealed places where a lack of knowledge was a factor in players' decisions not to report concussion symptoms. We suggest that education efforts do not always translate into knowledge that shapes reporting behaviors. This aligns with findings from a large systematic review of adolescent athletes under-reporting of concussion; the authors concluded that prior knowledge and education efforts do not necessarily deter under-reporting (PENNOCK et al., 2020). One area that we found revealed this tension was the intrapersonal symptom checklist players used to anticipate potential concussions. Concussion symptoms were normalized in players' minds, and some believed symptoms would mirror earlier concussion experiences despite substantive education efforts in recent years. Furthermore, players were not certain about how to interpret symptoms, or whether those symptoms posed a further risk, especially when dealing with short lived concussion events. Players were not concerned about the potential to mask concussion symptoms with pain drugs, and they continued to perceive pressures to play that influenced their decisions. We imply that knowledge and awareness are not yet at a sufficient level. We wish to highlight the importance of continuing to develop concussion awareness and educational initiatives, redirecting focus toward these key areas of concern, and further assessment of these efforts. The importance of education relates directly to the CFL, but may also have practical utility in other contexts. We recommend that education efforts focus on increasing recognition that players may normalize symptoms, that symptoms can change in subsequent concussions, that pain masking drugs can play a role in symptom recognition or early return to sport, that short-lived concussion events are significant, that factors beyond severity of symptoms are important and pressures of athletic identity permeate sporting culture, and that pressures to play are prevalent, especially amongst younger players or players with less job security. [63]
Another interesting finding was that with active concussion spotters and side-line tests, players now expect to be assessed after big impacts. Theoretically, this could be a benefit if players start to assume concussion symptoms will be checked. They may create associations between being hit and concussion assessment and become more likely to assess themselves more often. However, some players described gaming the concussion protocols, and preparing themselves to bypass the concussion tests. Again, we suggest this points to a lack of concern about the risk of continuing to play, possibly due to uncertainty or a lack of knowledge about the risks. This knowledge is useful for encouraging extra vigilance by trainers with testing and intervention procedures, and for increasing awareness of players themselves. [64]
We have added to the conversation about why CFL players may not be reporting their concussions and we contributed to knowledge about underreporting in different levels of sport. Some of our findings parallel existing research that documents under-reporting concussion in sport due to not wanting to stop playing, appearing weak to teammates (or coaches), letting teammates down, or losing a spot in the line-up (CHRISMAN et al., 2013). We expand on these ideas by also highlighting concerns about how players may normalize symptoms, expect symptoms to mirror previous concussion experience, be vulnerable to perceived pressures, feel pressure to present a resilient athletic identity, expect third-party assessment, and fail to recognize dangers of pain masking drugs. We also made visible uncertainties during self-assessment such as difficulty identifying symptoms, the uncertainty about a player's career, and the uncertainty of the risks of continued participation, all of which contribute to a context that encourages players to gamble with their health. [65]
The underreporting of concussion symptoms is highly relevant to current sport and education policy in the CFL and beyond, and is an important topic for future research. Concussion symptoms will always need to be reported by the player, as spotters and team trainers cannot always see and predict high impact events. An understanding of how pain masking drugs may interfere with a player's ability to recognize symptoms is an important area for future attention. Toradol was a commonly discussed pain killing drug, reportedly also used routinely by NFL players, and college level athletes (DUNNE, 2017). As Toradol is a drug that is often prescribed for symptoms of concussions such as pain relief and chronic migraines (GELFAND & GOADSBY, 2012), further research into this area and the masking of concussion symptoms is warranted. [66]
It would be beneficial if we could change prevalent attitudes toward valorization of athletes who report concussion symptoms rather than those who do not, and toward recognition that such an athlete will ultimately be the more reliable team player, compared to those who hide symptoms and potentially damage themselves. Perceived pressure to maintain one's athletic identity, more specifically to continue to play despite injury, and to show oneself as a resilient player is a common theme that is widespread across various sports. LISTON, McDOWELL, MALCOLM, SCOTT-BELL and WADDINGTON (2018) discussed how rugby union players held an irreverent attitude towards concussion which they termed "head strong" that ignored the significance of concussion and promoted risky behaviors. One player in our study discussed the stigma that still exists with concussion, calling it the "elephant in the room". People who are stigmatized may anticipate certain reactions from others, which aligns with our findings of players internalizing external pressures. We believe this implies a kind of double messaging that may be confusing to players. On one hand, the culture normalizes pain and the masking of pain, as "part of the game." As such it valorizes those who push past pain in the interests of the team and supports conformity to this sporting culture. On the other hand, the culture also states that it takes concussion seriously. Nonetheless, a sporting culture that accepts and promotes pain as part of the game promotes a situation whereby players are rewarded for underreporting concussion symptoms. Furthermore, it fuels conditions where teammates will not intervene when they suspect another player has a concussion. Athletes in this study worried about the downstream effects of reporting of concussion on a player's career. This aligns with other sport contexts, where it has been shown that management of concussion often fails to place concussion safety over career safety. MALCOLM (2009) discussed that doctors and physiotherapists avoided diagnosing concussion or using the term concussion unless absolutely certain, out of fear of jeopardizing athletes playing time. The question should be asked, why is it not universally valued for athletes to return to sport as healthy as possible, rather than risk a second impact, and long-term consequences such as neurocognitive decline? Serious brain injuries can have long lasting impacts on athletes' lives, as eloquently discussed in SMITH's (2008) story of her lifelong recovery from a traumatic brain injury (TBI). Focusing on the factors identified in this research related to perceived pressures to play—such as job security, importance of the game, and lifelong goals—may help players to become more explicitly aware of the issues. However, players continue to need support from their teammates, coaches, training staff, and sporting leagues to change the culture of concussion symptoms reporting to one that values health and offers tangible support to players throughout their recovery processes. One participant stated that reporting any concussion symptoms meant a "minimum of two weeks" off. This could have an effect on the need for certainty when self-assessing symptoms, and was demonstrated in the unwillingness to report a "potential" concussion, given that any symptoms could result in a two-week concussion protocol. This is different from other injuries where athletes may have a slight injury and may get an initial look, and be cleared to play, even if they brought the symptom to the attention of the trainer themselves. A sprained ankle can be played on until the player decides it is too severe, but a concussion does not have the same leeway. While it is not suggested to reduce these precautions, perhaps a policy change that would allow for return to play opportunities as warranted would have an effect on these decisions not to report symptoms. [67]
Players reading this information may find resonance with the results and compare their own experiences with those reported here. This could raise awareness and contribute to more informed decision-making about reporting symptoms. Similarly, athletes, trainers and policy makers in sporting leagues may find transferability of the themes discussed within this research to other contexts. Ultimately creating awareness of these issues involves connecting with the people involved. MALCOLM (2018) suggests reaching out to players' associations that are responsible for the protection of the athletes, as well as to brain injury organizations that petition for increased concern about concussions. To this end the Canadian Football League Players' Association, as well as relevant concussion and brain injury organizations and initiatives, should be made aware of these findings. [68]
In conclusion, a preliminary grounded theory is proposed that depicts stages, processes and factors related to reporting concussion symptoms, drawing on the accounts of ten Canadian Football League players. The authors hope that this work will advance understandings in the field and contribute to players', teammates', coaches', training staff's and the league's knowledge about, and responses to concussion symptoms. [69]
We would like to especially thank the ten athletes for their engagement in this project. Without their enthusiasm and willingness to openly share their experiences, this research would not be possible. We are also indebted to all of those who assisted with the recruitment process.
Anderson, Tim; Heitger, Marcus & Macleod, Angus D. (2006). Concussion and mild head injury. Practical Neurology, 6(6), 342-357, https://doi.org/10.1136/jnnp.2006.106583 [Accessed: December 9, 2018].
Bryant, Antony (2009). Grounded theory and pragmatism: The curious case of Anselm Strauss. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 10(3), Art. 2, https://doi.org/10.17169/fqs-10.3.1358 [Accessed April 7, 2021]
Casson, Ira R.; Viano, David C.; Powell, John W. & Pellman, Elliot J. (2010). Twelve years of national football league concussion data. Sports Health: A Multidisciplinary Approach, 2(6), 471-483.
CFL (2016). CFLPA announce new player health and safety measures. CFL, April 28, https://www.cfl.ca/2016/04/28/cfl-announces-new-player-health-and-safety-measures/ [Accessed: February 6, 2020].
Charmaz, Kathy (2002). Qualitative interviewing and grounded theory analysis. In Jaber F.Gubrium & James A. Holstein (Eds.), Handbook of interview research: Context and method (pp.675-694). London: Sage.
Charmaz, Kathy (2014). Constructing grounded theory (2nd ed.). London: Sage.
Chrisman, Sara P.; Quitiquit, Celeste & Rivara, Frederick P. (2013). Qualitative study of barriers to concussive symptom reporting in high school athletics. Journal of Adolescent Health, 52(3), 330-335.e3.
Delaney, Jeffrey S.; Caron, Jeffrey G.; Correa, Jose A. & Bloom, Gordon A. (2018). Why professional football players chose not to reveal their concussion symptoms during a practice or game. Clinical Journal of Sport Medicine: Official Journal of the Canadian Academy of Sport Medicine, 28(1), 1-12, https://doi.org/10.1097/JSM.0000000000000495 [Accessed: December 9, 2018].
Delaney, Jeffrey S.; Lacroix, Vincent J., Leclerc, Suzanne & Johnston, Karen M. (2000). Concussions during the 1997 Canadian football league season. Clinical Journal of Sport Medicine : Official Journal of the Canadian Academy of Sport Medicine, 10(1), 9-14.
Dunne, Tyler (2017). The NFL's drug of choice. The Lab: Bleacher Report, January 11, https://thelab.bleacherreport.com/nfl-toradol-use-players-survey/ [Accessed: February 26, 2020].
Evers, Jeanine C. (2016). Elaborating on thick analysis: About thoroughness and creativity in qualitative analysis. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 17(1), Art. 6, https://doi.org/10.17169/fqs-17.1.2369 [Accessed April 7, 2020].
Fraas, Michael R.; Coughlan, Garrett F.; Hart, Emily C. & McCarthy, Conor (2014). Concussion history and reporting rates in elite Irish rugby union players. Physical Therapy in Sport, 15(3), 136-142.
Furness, Zack (2016). Reframing concussions, masculinity, and NFL mythology in league of denial. Popular Communication, 14(1), 49-57.
Galetta, Kristin M.; Brandes, Lauren E.; Maki, Karl; Dziemianowicz, Mark S.; Laudano, Eric; Allen, Megan; Sennet, Brian; Wiebe, Douglas; Devick, Steve; Messner, Leonard; Galetta, Steven L. & Balcer, Laura J. (2011). The king-devick test and sports-related concussion: study of a rapid visual screening tool in collegiate cohort. Journal of the Neurological Sciences, 309(1-2), 34-39.
Ganga, Deianira & Scott, Sam (2006). Cultural "insiders" and the issue of positionality in qualitative migration research: Moving "across" and moving "along" researcher-participant divides. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 7(3), Art. 7, https://doi.org/10.17169/fqs-7.3.134 [Accessed April 8, 2021].
Gelfand, Amy A. & Goadsby, Peter J. (2012). A neurologist's guide to acute migraine therapy in the emergency room. Neurohospitalist, 2(2), 51-59. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3737484/ [Accessed: February 26, 2020].
Goldberg, Daniel S. (2008). Concussions, professional sports, and conflicts of interest: Why the national football league's current policies are bad for its (players') health. HEC Forum, 20(4), 337-355.
Guskiewicz, Kevin M.; Marshall, Stephen W.; Bailes, Julian; McCrea, Michael; Cantu, Robert C.; Randolph, Christopher & Jordan, Barry D. (2005). Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery, 57(4), 719-726, https://doi.org/10.1093/neurosurgery/57.4.719 [Accessed: December 11, 2018].
Kelle, Udo (2005). "Emergence" vs. "forcing" of empirical data? A crucial problem of "grounded theory" reconsidered. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 6(2), Art. 27, https://doi.org/10.17169/fqs-6.2.467 [Accessed: April 8, 2021].
Kelly, Ethan (2017). National Football League concussions from 2009 – 2015: A secondary data analysis. The Young Researcher, 1(1), 27-36. http://www.theyoungresearcher.com/papers/kelly.pdf [Accessed February 12, 2021]
Kerr, Zachary Y.; Chandran, Avinash; Nedimyer, Aliza K.; Arakkal, Alan; Pierpoint, Lauren A. & Zuckerman, Scott L. (2019). Concussion incidence and trends in 20 high school sports. Pediatrics, 144(5), e20192180-e20192180, https://doi.org/10.1542/peds.2019-2180 [Accessed: February 12, 2021].
Lehman, Everett J.; Hein, Misty J.; Baron, Sherry L. & Gersic, Christine M. (2012). Neurodegenerative causes of death among retired national football league players. Neurology, 79(19), 1970-1974.
Liston, Katie; McDowell, Mark; Malcolm, Dominic; Scott-Bell, Andrea & Waddington, Ivan (2018). On being "head strong": The pain zone and concussion in non-elite rugby union. International Review for the Sociology of Sport, 53(6), 668-684.
Longworth, Thomas; McDonald, Andrew; Cunningham, Corey; Khan, Hussain & Fitzpatrick, Jane (2021). Do rugby league players under-report concussion symptoms? A cross-sectional study of elite teams based in Australia. BMJ Open Sport and Exercise Medicine, 7(1), 860, https://doi.org/10.1136/bmjsem-2020-000860 [Accessed: February 2, 2021].
Malcolm, Dominic (2009). Medical uncertainty and clinician-athlete relations: The management of concussion injuries in rugby union. Sociology of Sport Journal, 26(2), 191-210.
Malcolm, Dominic (2018). Concussion in sport: Public, professional and critical sociologies. Sociology of Sport Journal, 35(2), 141-148.
Manley, Geoff T.; Gardner, Andrew J.; Schneider, Kathryn J.; Guskiewicz, Kevin M.; Bailes, Julian; Cantu, Robert C.; Castellani, Rudolph J.; Turner, Michael; Jordan, Barry D.; Randolph, Christopher; Dvořák, Jiri; Hayden, Alix K.; Tator, Charles H.; McCrory, Paul & Iverson, Grant L. (2017). A systematic review of potential long-term effects of sport-related concussion. British Journal of Sports Medicine, 51(12), 969-977, https://doi.org/10.1136/bjsports-2017-097791 [Accessed: February 25, 2020].
May, Todd; Foris, Lisa A. & Donnally III, Chester J. (2020). Second impact syndrome. StatPearls, https://www.ncbi.nlm.nih.gov/books/NBK448119/ [Accessed: February 6, 2020].
McCrea, Michael; Hammeke, Thomas; Olsen, Gary; Leo, Peter & Guskiewicz, Kevin M. (2004). Unreported concussion in high school football players. Clinical Journal of Sport Medicine, 14(1), 13-17.
McCrory, Paul; Meeuwisse, Willem; Dvorak, Jiri; Aubry, Mark; Bailes, Julian; Broglio, Steven; Cantu, Robert C.; Cassidy, David; Echemendia, Ruben J.; Castellani, Rudy J.; Davis, Gavin A.; Ellenbogen, Richard; Emery, Carolyn; Engebretsen, Lars; Feddermann-Demont, Nina; Giza, Christopher C.; Guskiewicz, Kevin M.; Herring, Stanley; Iverson, Grant L.; Johnston, Karen M.; Kissick, James; Kutcher, Jeffrey; Leddy, John J.; Maddocks, David; Makdissi, Michael; Manley, Geoff T.; Putukian, Margot; Schneider, Kathryn; Sills, Allen; Tator, Charles H.; Turner, Michael & Vos, Pieter E. (2017). Consensus statement on concussion in sport—The 5th International Conference on Concussion in Sport held in Berlin, October 2016. British Journal of Sports Medicine, 51, 838-847, https://doi.org/10.1136/bjsports-2017-097699 [Accessed: December 9, 2018].
McPherson, April L.; Nagai, Takashi; Webster, Kate E. & Hewett, Timothy E. (2019). Musculoskeletal injury risk after sport-related concussion: A systematic review and meta-analysis. American Journal of Sports Medicine, 47(7), 1754-1762.
Meier, Timothy B.; Brummel, Bradley J.; Singh, Rashmi; Nerio, Christopher J.; Polanski, David W. & Bellgowan, Patrick S.F. (2015). The underreporting of self-reported symptoms following sports-related concussion. Journal of Science and Medicine in Sport, 18(5), 507-511.
Moreau, Matthew S.; Langdon, Jody & Buckley, Thomas A. (2014). The lived experience of an in-season concussion amongst NCAA division I student-athletes. International Journal of Exercise Science, 7(1), 62-74, https://digitalcommons.wku.edu/ijes/vol7/iss1/8 [Accessed: June 5, 2016].
Naidu, Dhiren; Borza, Carley; Kobitowich, Tara & Mrazik, Martin (2018). Sideline concussion assessment: The King-Devick test in Canadian professional football. Journal of Neurotrauma, 35(19), 2283-2286.
Oltmann, Shannon M. (2016). Qualitative interviews: A methodological discussion of the interviewer and respondent contexts. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 17(2), Art. 15, https://doi.org/10.17169/fqs-17.2.2551 [Accessed: April 7, 2021].
Patton, Michael Q. (2002). Qualitative research & evaluation methods (3rd ed.). London: Sage.
Pennock, Kaleigh F.; McKenzie, Braeden; Steacy, Laura M. & Mainwaring, Lynda (2020). Under-reporting of sport-related concussions by adolescent athletes: A systematic review. International Review of Sport and Exercise Psychology, 1-27.
Ramalho, Rodrigo; Adams, Peter; Huggard, Peter & Hoare, Karen (2015). Literature review and constructivist grounded theory methodology. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 16(3), Art. 19, https://doi.org/10.17169/fqs-16.3.2313 [Accessed April 8, 2021].
Register-Mihalik, Johna K.; Guskiewicz, Kevin M.; McLeod, Tamara C.V.; Linnan, Laura A.; Mueller, Frederick O. & Marshall, Stephen W. (2013). Knowledge, attitude, and concussion-reporting behaviors among high school athletes: A preliminary study. Journal of Athletic Training, 48(5), 645-653. https://doi.org/10.4085/1062-6050-48.3.20 [Accessed: June 5, 2016].
Russell, Glenda M. & Kelly, Nancy H. (2002). Research as interacting dialogic processes: Implications for reflexivity. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 3(3), Art. 18, https://doi.org/10.17169/fqs-3.3.831 [Accessed: April 7, 2021].
Smith, Claire (2008). Performing my recovery: A play of chaos, restitution, and quest after traumatic brain injury. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 9(2), Art. 30, https://doi.org/10.17169/fqs-9.2.410 [Accessed: April 7, 2021].
Thornberg, Robert & Charmaz, Kathy (2014). Grounded theory and theoretical coding. In Uwe Flick (Ed.), The Sage handbook of qualitative data analysis (pp.153-169). London: Sage.
Ventresca, Matt & McDonald, Mary G. (Eds.) (2019). Sociocultural examinations of sports concussions. New York, NY: Routledge.
Daryl William Harrison STEPHENSON is an adjunct professor at Western University. He holds a PhD in health and rehabilitation sciences from Western University and a master's degree in human kinetics from the University of Windsor. He currently works for the Occupational Health Clinics for Ontario Workers in Hamilton Ontario Canada.
Contact:
Daryl William Harrison Stephenson
Western University, Health and Rehabilitation Sciences
London, Ontario, N6A 3K7, Canada
E-mail: dstephe@uwo.ca
Elizabeth Anne KINSELLA is a professor in the Institute of Health Sciences Education, Faculty of Medicine and Health Sciences, at McGill University. She is interested in health professions education, knowledge mobilization in health and social care, human occupations, ethics, praxis, and qualitative research.
Contact:
Elizabeth Anne Kinsella
McGill University, IHSE, Faculty of Medicine & Health Sciences
1110 Pine Avenue West, Lady Meredith House, Montreal, Quebec, Canada, H3A 1A3
E-mail: elizabeth.kinsella@mcgill.ca
URL: https://sites.google.com/site/akinsell/home
Jeffrey David HOLMES is an associate professor at Western University. His research interests are in concussion education, management and psychosocial implications on occupational identity, non-pharmacological management of gait and balance impairments among individuals with Parkinson's disease, evaluation of novel treatments, diagnostic procedures, and teaching practices in occupational therapy.
Contact:
Jeffery David Holmes
Western University, Health and Rehabilitation Sciences
London, Ontario, N6A 3K7, Canada
E-mail: jholme@uwo.ca
URL: https://www.uwo.ca/fhs/ot/about/faculty/holmes_j.html
Andrew Malcolm JOHNSON is currently the acting director for the School of Health Studies at Western University. His primary research interests relate to the identification of patient values within an evidence-based practice framework, methods for identifying concussions, and the tracking of concussion symptoms.
Contact:
Andrew Malcolm Johnson
Western University, School of Health Studies
London, Ontario, N6A 3K7, Canada
E-mail: ajohnson@uwo.ca
URL: https://www.uwo.ca/fhs/shs/about/faculty/johnson_a.html
Stephenson, Daryl William Harrison; Kinsella, Elizabeth Anne; Holmes, Jeffrey David & Johnson, Andrew Malcolm (2021). Canadian Football League Players' Reporting of Concussion Symptoms [69 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 22(2), Art. 16, http://dx.doi.org/10.17169/fqs-22.2.3615.